It wasn’t too long ago that the term microbiome seemed to imply a singular entity that took up residence in the gut. However, it has become increasingly clear that the human microbiome is not just confined to the gut, but in fact stretches head to toe, inside and out.
While understanding the gut microbiome is important, it has also become clear that our niche microbiomes - from the gut to the skin to the mouth - are not only helping each specific area function separately but also as a unified whole. And while these microbes specialize, they also roam and travel, impacting your whole health. Case in point: the oral microbiome.
Let's dig deep with Dr. Jesse Myers, Doctor of Dental Medicine, and get A’s to some of the most pressing Q’s on the oral microbiome, its impact on general health, and how you can improve both.
Q: First things first: why is oral health so important?
A: That's a really timely question. In this day and age, I feel like it's one of the major missing puzzle pieces in the complete picture of health and wellness. To start from just a visual perspective, your teeth are one of the first things that people notice about you. A healthy smile is oftentimes a source of self-confidence for people, and in turn, it can affect your mental health. I know that this was true for myself. Before I had braces, I was unmotivated, lacking in self-belief, and I wasn't thriving. The power of a smile completely changed my world and gave me motivation to pursue my dreams.
But your relationship to oral health is about much more than aesthetics, with strong links to systemic health. In fact, poor dental health is directly linked to diabetes, Alzheimer's disease, and cardiovascular diseases to name a few.
Further, in medicine, we often compartmentalize the body into individual components. We really miss the big picture and lose sight of the whole; we lose sight that the body is more than just the sum of its simple parts. It's one functioning system, not in isolation. And a lot of these direct links to systemic issues are mediated through the oral microbiome, or should I say, an imbalance in the oral microbiome.
Q: Why is the oral microbiome so important?
A: So, just like the gut has its own microbiome, the mouth has its own niche biome known as the oral microbiome. The oral microbiome is a term that encapsulates the entirety of all the different microorganisms that are living inside of the mouth, including bacteria, fungi, archaea, and viruses. In fact, the mouth is the second most highly populated area right after the gut. It’s full of diversity, and it’s a very unique habitat. And even within the oral environment, there are all these different habitats or niches that the microbiome lives on, including the teeth, the tongue, the mucosal surfaces of our cheeks, and around the gums.
Generally speaking, the oral microbiome acts as a gatekeeper, protecting us against intruders and invader species. Just by occupying space, these microbes prevent and out compete pathogenic bacteria that might be contributing to systemic inflammation. Through that mechanism alone, they prime our immune systems to recognize friend from foe. So, these microbes play a major role in helping our immune systems mount the proper types of responses.
And not only that, but they also protect all the surfaces that are inside of our mouth, including our teeth. In fact, plaque is exactly that: microbes on the teeth. The oral microbiome likes to live in these communities called biofilms. And that biofilm, or the plaque that's on your teeth, is actually where you get this protective insulating layer, depending on the composition of that microbiome.
But one of the really exciting discoveries that we've made about the oral microbiome specifically has to do with the ability of bacteria in the mouth to metabolize nitrogen compounds. The oral microbiome helps to heal and rebuild our teeth, or the outer surface of the enamel. And this is occurring through a pathway called the arginine deiminase system.
Arginine is one of the essential amino acids that we will typically find in poultry, red meat, fish, eggs, etc. and this amino acid has nitrogen within it. And what certain bacteria in the mouth will do is they'll take this amino acid, L arginine, into their own cells and they will convert it into alkali products which helps to raise the pH in the mouth and neutralize any acidity, which will then help to deliver calcium or minerals into the teeth.
We've always thought that these bacteria in the mouth are what was causing tooth decay. And now we realize that they're actually playing a major role in protecting us and healing our teeth.
Q: Does this mean that plaque is, in fact, good?
A: It really depends on the composition. Plaque can definitely contribute to disease. And some examples of an imbalance in the oral microbiome include gum diseases like gingivitis, or periodontal disease, bleeding gums, red swollen gums, along with potential bone destruction. What will happen in these situations is that there's a heavier plaque that gets built up. And the types of bacteria that are inside of that plaque are bacteria that are thriving in poor conditions. And that plaque ends up getting straight-line access into the bloodstream and can wreak havoc. So, essentially it depends on the type of microbiome that you are cultivating. Composition is key.
Q: What about digestion? Is it true that microbes start digesting food in the mouth?
A: Yeah, chewing your food is really the first part of our digestive system. We have the ability to break down complex proteins, complex carbohydrates, and fiber, right here in the mouth. And a lot of times we completely forego that first part of the digestive system, a lot of which is due to the softer foods that we're eating as part of a modern diet. So, we don’t even chew with our teeth as much as we used to. And, by chewing with our teeth, we're able to produce more saliva, which helps to break down food even further.
Another thing is that we're not getting into that parasympathetic activation, or the rest and digest, when we eat as much as we should. Part of that is because we're not consciously and intentionally eating our food and spending time with it, enjoying it, being able to taste it. And it primes our entire body for improper digestion, because we're still in a fight or flight, or sympathetic nervous system activation. So, something I'll do is consciously try to chew my food, while enjoying the taste of it, and breathing through my nose, which will also assist with creating nitric oxide, and allowing my body to deliver nutrients properly.
Q: Are there any telltale signs of an imbalanced oral microbiome?
A: Cavities are really one of the best examples of oral microbiome dysbiosis. In fact, they are the most common chronic disease that is experienced worldwide, especially in the United States. So, if you have a cavity, you likely have some form of oral microbiome dysbiosis that should be looked further into.
There's a study1 that was just released in 2021 that evaluated SIBO, which stands for small intestinal bacterial overgrowth. It's a major GI distress disease that we're seeing where bacteria are thought to migrate up from the large intestines into an area within the small intestines, where you're not supposed to have a high abundance of bacteria.
This study used endoscopies, (which is basically where we put a telescope down the throat to investigate the gut). What they found was that 89% of the bacterial composition of these patients that had SIBO matched the bacteria that was in the mouth and in the saliva.
So, you're constantly swallowing the oral microbiome (and you’re producing around one liter of saliva a day). But, if you have bleeding gums, Gingivitis, or periodontal disease, all those bacteria are getting straight-line access into the bloodstream and priming the body for permanent autoimmune attacks.
One of the notorious bacteria that we find frequently in high abundance in periodontal disease is called porphyromonas gingivalis, or P. gingivalis. This type of bacteria has two virulence factors (traits) that make it toxic.
First, the cell membrane has an LPS (or lipopolysaccharide), that causes endotoxemia (which causes low-grade inflammation). And then there are also these little enzymes that they produce called gingipains. And we're starting to see that not only the presence of this bacteria, but the presence of LPS and gingipains is directly linked to causing heart attacks, degrading the tight junctions that are, really anywhere in the body, but specifically in the cardiovascular system.
But one of the most recent things that we have found is that P. gingivalis has also been discovered in the brains of Alzheimer's disease patients. So, we're starting to shift our attention away from the amyloid beta hypothesis (which relates the cause of Alzheimer's disease to the presence of amyloid beta plaques in the brain) and seeing that the gingipains, LPS, and the presence of P. gingivalis is causing an inflammatory response in the brain. It's actually thought now that the amyloid beta plaques are an antimicrobial response to these bacteria that we find in the mouth.
Learn more by reading about the Gut-Brain Axis
Q: So, where does antimicrobial mouthwash fit into the oral microbiome picture?
A: There are a few issues with antimicrobial mouthwashes. For starters, the pH is acidic and can cause your tooth structure to break down. But even more detrimentally, these mouthwashes can disrupt nitric oxide production.
The oral microbiome is one of the key players making the miraculous communicating molecule called nitric oxide. How this happens is that there's certain oral bacteria that will take nitrates out of saliva and then take them into the nitric oxide pathway. And we've discovered this by seeing what antibacterial mouthwashes will do to the oral microbiome, which will completely knock out the nitrogen metabolism that these bacteria do for us.
In fact, there was a study2, I believe in 2019, where they took healthy individuals and had them do cardiovascular intensive exercise on a treadmill. And something that exercise does for us (which is really medicine), is all the way up until two hours after workout, we have this physiological response called post exercise hypotension, where we get this blood pressure lowering effect, and that is basically mediated by nitric oxide. So nitric oxide will help open our blood vessels and dilate them and allow us to have optimal delivery of oxygen and nutrients to the whole body.
So, right after these athletes did this intense workout, they swished with something called Chlorhexidine mouthwash, which is one of dentistry’s gold standard treatments for periodontal disease, gingivitis, and cavities. What they saw was that these athletes’ blood pressures skyrocketed. And all the way up until two hours after they had an attenuation, or weakening, of the ability of bacteria to create nitric oxide for us.
And yet, around 40% of Americans are swishing with antibacterial mouthwashes like Chlorhexidine3. But also, people are frequently using Listerine, which is a low antibacterial mouthwash. And we've now seen studies4 (observational, not causal) that have evaluated a particular subset of the human population that are overweight or obese, but they don't currently have high blood pressure or diabetes. And after three years, following up with these patients, they saw that individuals who swished with over-the-counter mouthwash more than two times a day, went on to develop hypertension, prediabetes, or diabetes. After multivariate analysis that accounted for other risk factors, they still found that frequent use of antiseptic mouthwash was an independent risk factor.
So, I no longer suggest that people use antibacterial mouthwashes because of this key role that oral bacteria play in our overall wellbeing. You're basically indiscriminately nuking the good along with the bad bacteria. And the bacteria that can thrive in poor conditions are the ones that are going to come back.
Q: What can we do to promote a balanced oral microbiome?
A: Well, nutrition is one of the most easily obtainable things that you can use to protect yourself. So, cultivating an awareness of the types of things that you're putting into your body is first and foremost. Maintaining a nutrient-dense diet and feeding the microbiome food rich in compounds called nitrates (found in leafy greens like arugula) is where a lot of this work begins.
I also think one of the most protective things that you can do is reduce the amount of refined carbohydrates and free sugars that you are eating daily. On a daily basis, the average American is eating 77 grams of sugar. That's around 17 to 25 teaspoons of sugar and not always in sucrose. Refined carbohydrates, like white processed flour, crackers, sugary, sweetened drinks, and alcohol are where we're getting a major source of these sugars.
The oral microbiome can shift towards dysbiosis by the amount and frequency at which these free sugars and carbohydrates are getting into the body. And fungal species, as well as specific bacterial species within the genus streptococcus, along with the key players in gingival inflammation, will thrive in an environment that's high in these free sugars. Cavities and gum diseases simply don't happen in the absence of sugar.
In fact, there's this great study from the Journal of Periodontology called The Impact of Gingival Conditions in the Absence of Oral Hygiene5. What they did was take people out into the wilderness (like the TV show Alone or Survivor), and they didn't give them floss or toothbrushes or toothpaste. They essentially tried to mimic a hunter-gatherer diet and they spent about a month just kind of living this lifestyle. What they noticed was that there weren't any cavities, there weren't gum diseases, and their indices of health improved. They saw that the oral microbiome increased in its diversity, and the number of bacteria grew. They concluded that cavities and gum diseases aren’t occurring in the absence of refined carbohydrates.
It's important for us to cultivate the understanding that sucrose and a diet that's high in refined carbohydrates is priming our bodies for inflammation and disease. And while it starts in the mouth, that inflammation spreads everywhere.
Q: It’s almost as if modern dental health is worse than that of primitive man. Is this due in large part to imbalanced microbiomes and too much sugar?
A: Yeah, when we look at the anthropological records of hunter-gatherer societies, we can study calculus (hardened plaque on the backside of teeth) from ancient societies. The fossilized microbiomes found inside of those dental calculus are well preserved. Modern man has shifted to a cariogenic microbiome, which is a microbiome that causes cavities and gum diseases. Our ancestors just didn't have these issues.
Q: There truly does seem to be a wisdom in nature’s design when it comes to health that we just cannot replicate.
A: Humans are holobionts (or living, walking ecosystems, like a rain forest). Being outside in nature, and being in touch with nature, is just how we're designed to live. And this nature has everything to do with the type of microbiomes that we're cultivating within us. I try to get outside and into nature, multiple times a week, to regulate my nervous system and get my body back in touch with how things should be.
Q: Switching gears a little, what’s your perspective on nasal breathing? Can this benefit oral health?
A: Yes. Personally, something I do to promote nasal breathing on a nightly basis is I mouth tape. And one of the reasons I do that is because saliva should constantly be bathing your mouth, and your teeth. It has a protective role of being able to wash away bad bacteria. It also allows the immune system to bathe our teeth. And if you are mouth breathing, you are causing a shift in the microbiome of the mouth to go towards acidity. So, over the course of time, this can contribute to cavities.
But really, the major thing that I'm concerned with as a doctor, is sleep apnea. And people that have chronic obstructive sleep apnea are mouth breathers. And we see that sleep apnea is linked to strokes, heart attacks, Alzheimer's disease, and just widespread inflammation throughout the body.
So, I'm a major proponent of trying to get people to start breathing through their nose again, because of its vital importance (especially for young kids as it allows for proper facial development and growth).
Learn more about nasal breathing
Q: If there was just one piece of advice you could give a patient, what would that be?
A: Well, it would be threefold. First and second, I'm still a big believer in brushing and flossing your teeth, traditional dentistry that is tried and true, especially as microbiome science is being applied to the dental field. Mechanically, removing the plaque and some of these bad bacteria is one of the best ways that you can try to cultivate a good oral microbiome.
If the mouth is a verdant garden, there are always going to be roles for the weeds in the garden. But you never want the weeds to choke out the fruit bearing plants. And so, you have to constantly maintain that garden. Brushing and flossing are still major lifestyle habits that you can cultivate to protect yourself.
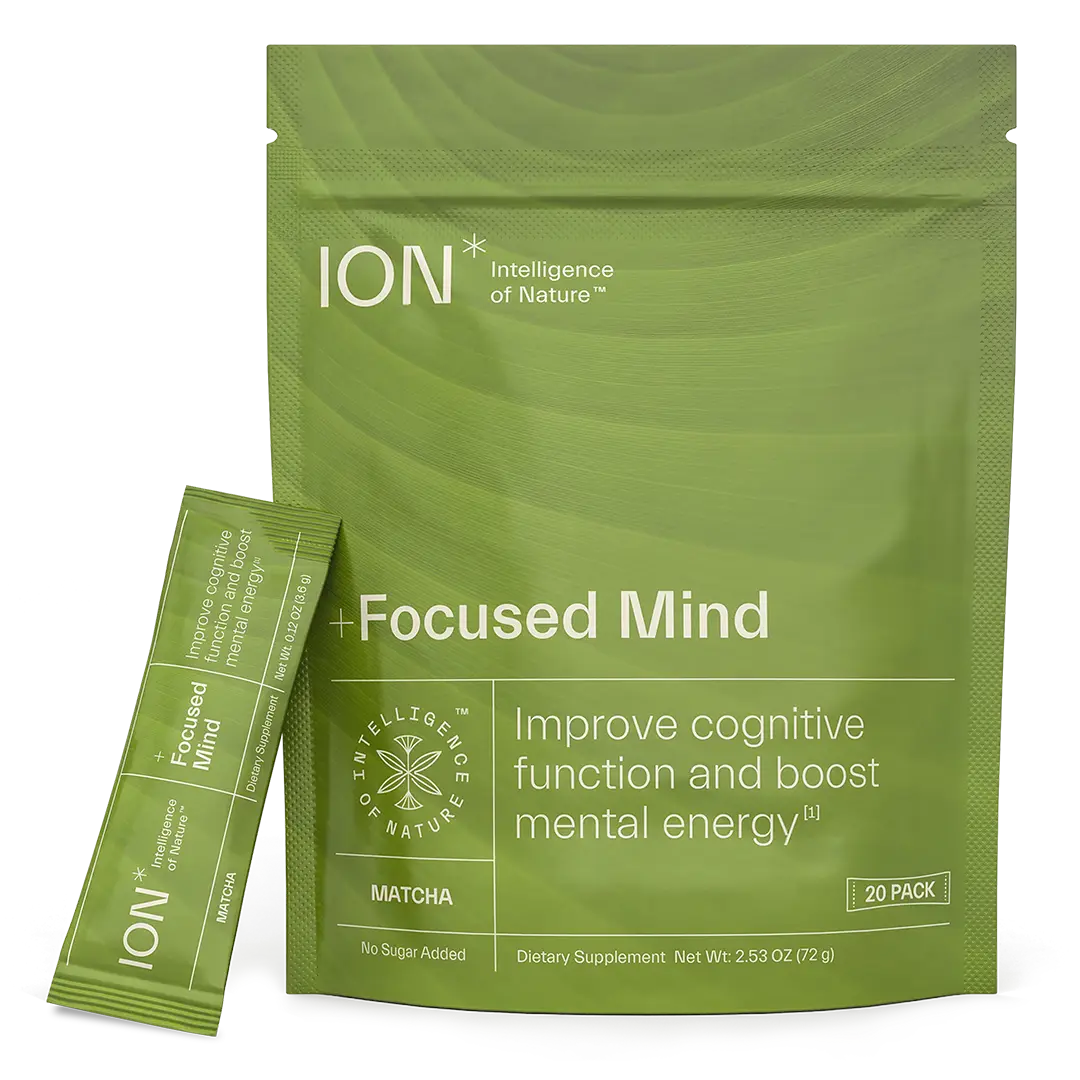
And third, again, just really starting to maintain an awareness of the food that you're putting into your body and how that's affecting this whole ecosystem. I would also say, for anybody who is using ION* Gut Support or thinking about investing in your health, you should be using as a mouthwash as well, swishing with it for a minute and really getting it in between your teeth.
Similar to how ION* Gut Support can assist with strengthening the gut lining by increasing tight junction expression, I believe it can also help assist with leaky gums. I believe it has the potential to help protect those tight junctions that exist in the mouth and start facilitating a balanced microbiome at the start of the digestive process.

Dr. Jesse Myers is a Doctor of Dental Medicine practicing in Staunton Virginia. He is a functional dentist who integrates food as medicine and lifestyle suggestions for optimal health into modern dentistry. Dr. Myers is passionate about shedding light on how complete whole-body health starts in the mouth.
References:
- Barlow JT, Leite G, Romano AE, et al. “Quantitative sequencing clarifies the role of disruptor taxa, oral microbiota, and strict anaerobes in the human small-intestine microbiome”. Microbiome. 2021; 9(1):214. Published 2021 Nov 2. doi:10.1186/s40168-021-01162-2
- Cutler C, Kiernan M, Willis JR, et al. “Post-exercise hypotension and skeletal muscle oxygenation is regulated by nitrate-reducing activity of oral bacteria”. Free Radic Biol Med. 2019; 143:252-259. doi:10.1016/j.freeradbiomed.2019.07.035
- Joshipura K, Muñoz-Torres F, Fernández-Santiago J, Patel RP, Lopez-Candales A. “Over-the-counter mouthwash use, nitric oxide and hypertension risk”. Blood Press. 2020;29(2):103-112. doi:10.1080/08037051.2019.1680270
- Joshipura KJ, Muñoz-Torres FJ, Morou-Bermudez E, Patel RP. “Over-the-counter mouthwash use and risk of pre-diabetes/diabetes”. Nitric Oxide. 2017;71:14-20. doi:10.1016/j.niox.2017.09.004
- Baumgartner S, Imfeld T, Schicht O, Rath C, Persson RE, Persson GR. “The impact of the stone age diet on gingival conditions in the absence of oral hygiene”. J Periodontol. 2009;80(5):759-768. doi:10.1902/jop.2009.080376